If a dentist recommends root canal treatment, there’s no need to panic. Modern endodontic care focuses on relieving pain and preserving your natural tooth whenever possible. Root canal therapy is a predictable, conservative solution when the inner tissues of a tooth—known collectively as the dental pulp—have been damaged by decay, trauma, or infection.
At the office of Lesley Holloway the Dentist in Laurel, NE, we combine careful diagnosis with gentle techniques to make the process as comfortable and straightforward as possible. Our team will explain your options and guide you through every step so you can make informed choices about your oral health.
Retaining a natural tooth whenever feasible is usually the best long-term outcome for both function and appearance. A tooth that has been maintained with root canal therapy continues to support adjacent teeth, preserves the jawbone, and helps you chew and speak without the limitations that sometimes come with tooth replacement options.
Root canal therapy addresses the problem at its source by removing diseased tissue from inside the tooth and sealing it to prevent reinfection. When paired with an appropriate restoration, this approach often restores strength and stability so the tooth can last for many years — frequently for the remainder of a patient’s life with proper home care and routine dental maintenance.
Success rates for modern root canal procedures are high when performed with careful technique and follow-up care. The decision to treat rather than extract a tooth considers many factors, including how much healthy tooth structure remains, the tooth’s strategic value in the bite, and overall periodontal support.

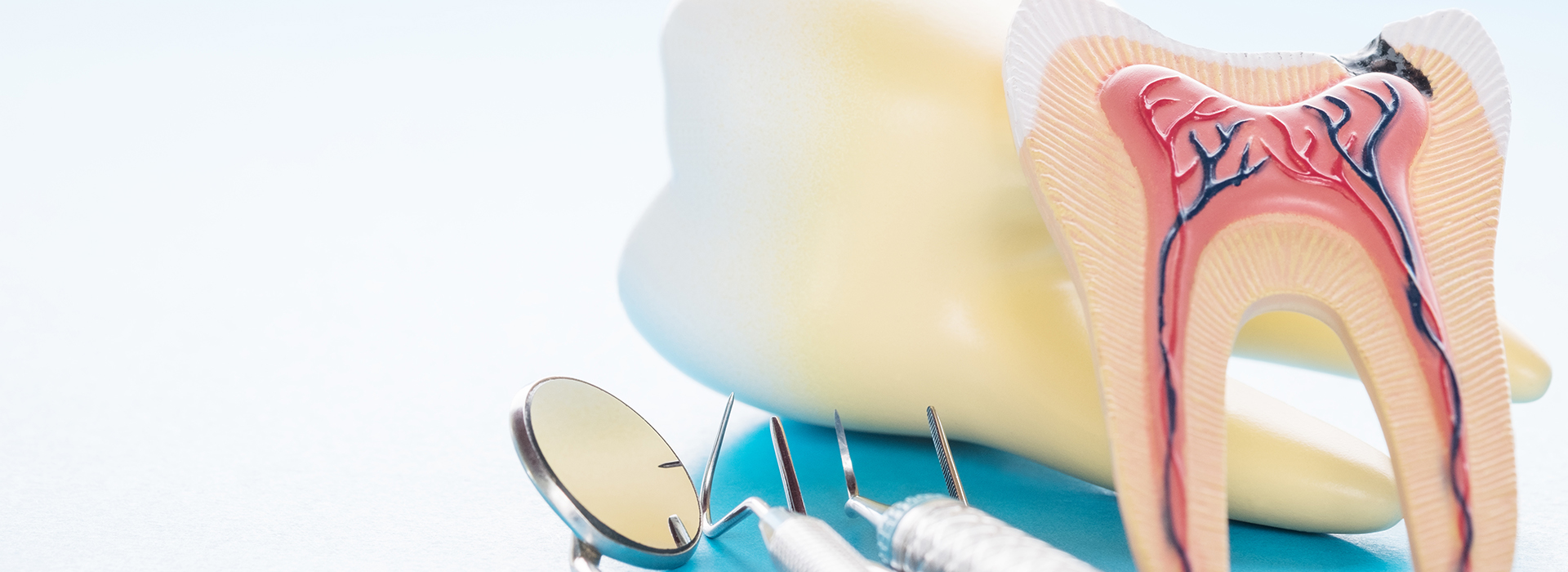
Inside every tooth is a small chamber containing the pulp — a combination of nerve fibers, blood vessels, and connective tissue. When bacteria reach this internal space through deep decay, cracks, or trauma, the pulp can become inflamed or necrotic. That internal breakdown is what often leads to the symptoms that bring patients in for evaluation.
Symptoms can vary. Some people feel severe, lingering pain or sharp sensitivity to hot and cold. Others notice a darkening of a tooth, swelling of the gum, or discomfort when biting. In other cases, there may be no obvious symptoms and, the problem is detected only on an x-ray during a routine exam. Careful assessment and imaging help determine whether root canal therapy is the appropriate course.
A tooth needing root canal treatment isn’t automatically unsalvageable. If enough healthy structure remains and the surrounding bone and gum tissue are stable, root canal therapy can remove the source of infection and allow the tooth to be restored and preserved in the long term.
Not every ache signals the need for a root canal, but certain patterns raise concern and warrant a prompt dental evaluation. Persistent or worsening pain—especially pain that disrupts sleep or comes on without an obvious trigger—should be assessed without delay. Pain that lingers after exposure to temperature changes is another common indicator of pulp involvement.
Other signs include visible discoloration of a tooth after injury, swelling or tenderness in the gum near the tooth, and sensitivity when biting down. Sometimes a chronic infection drains slowly and causes intermittent discomfort rather than a dramatic, acute episode; this underscores importance of routine exams and x-rays to catch problems early.
When signs point to pulpal disease, our approach is to confirm the diagnosis using clinical tests and radiographs, discuss the findings openly with you, and recommend a treatment plan tailored to the tooth and your broader oral health goals.
Unrelenting tooth pain, pain that wakes you at night, or pain that grows worse over several days generally indicates an advancing problem. In many instances, root canal treatment is the most effective way to remove the source of pain and protect the surrounding tissues.
Intense sensitivity to hot or cold foods and drinks—especially when the sensation lingers—suggests inflammation or compromised nerve tissue inside the tooth.
Pain when biting or a feeling of something being “off” when you chew can indicate that the internal tissues are affected or infection has reached the root tip.
A tooth that darkens after a blow or gradually discolors over time may have lost its internal vitality, signaling a problem that requires evaluation.
Cracked or fractured teeth can expose inner tissues to bacteria and trauma. If the damage is deep enough to reach the pulp, root canal therapy can often save the tooth.
Localized swelling or an abscess with drainage is a sign that an infection has progressed. Prompt treatment reduces the risk of more serious complications.
If infection has damaged the supporting bone, the affected tooth may feel loose. Treating the source of infection can allow healing and stabilization in many cases.

Delaying care after the pulp has been compromised increases the chance that an infection will spread and cause greater damage to the tooth and surrounding structures. Early intervention limits the extent of treatment needed and reduces the likelihood of more invasive procedures later on.
Some teeth with pulpal problems remain quiet for a period and are only identified during routine exams or on x-rays. When a problem is caught before extensive destruction occurs, the prognosis is generally better and, restoration is more predictable.
Our priority is to assess each situation promptly and recommend a thoughtful plan. We’ll explain expected outcomes, restoration needs, and follow-up care so you know what to expect and can move forward with confidence.
Modern root canal therapy is performed with attention to comfort and precision. After numbing the area, the dentist gains access to the pulp chamber, gently removes diseased tissue, and shapes the canals so they can be cleaned and disinfected. Advanced instruments and materials help ensure the canals are thoroughly prepared before sealing.
Some teeth are straightforward and can be treated in a single visit; others—particularly those with complex anatomy or active infections—may require two appointments to allow for thorough disinfection. The length and number of visits depend on each tooth’s unique needs.
Once the canals are sealed with a biocompatible filling material, the tooth is typically rebuilt with a permanent restoration. A full-coverage crown is often recommended for back teeth to protect them from fracture and restore full chewing function. If additional relaxation is needed for anxious patients, sedation options are available and can be discussed in advance.

After your procedure, mild soreness or tenderness is common for a few days as the surrounding tissues heal. Over-the-counter pain relievers usually manage this discomfort comfortably; we’ll provide clear instructions for post-operative care and any prescriptions if indicated.
Protecting the treated tooth while a final restoration is planned is important. Temporary fillings or build-ups are effective in the short term, but the long-term success of the treatment usually depends on placing a well-fitting permanent restoration to prevent fracture or recontamination.
Good oral hygiene and regular dental checkups are essential to monitor healing and ensure lasting success. With careful restoration and routine maintenance, a tooth that has received root canal therapy can function well for many years — often a lifetime.
At our Laurel office, patient comfort and clear communication guide every treatment decision. If you think you may need root canal care or you’re experiencing symptoms described here, we’re here to help.
To learn more about root canal therapy or to discuss your situation, please contact us for additional information and to schedule an evaluation.
A root canal is a dental procedure that removes infected or inflamed pulp from inside a tooth and seals the space to prevent reinfection. The pulp contains nerves and blood vessels that can become compromised by deep decay, cracks, or trauma, causing pain and potential spread of infection. Root canal therapy is recommended when the pulp cannot recover on its own and preserving the natural tooth offers better long-term function than extraction.
When successful, root canal treatment eliminates the source of pain and allows the tooth to remain in the mouth, supporting chewing function and adjacent teeth. The decision to proceed is based on clinical exam and imaging to assess the extent of damage and the tooth's structural viability. At the office of Lesley Holloway the Dentist in Laurel, NE, we evaluate each case and explain why root canal therapy may be the most predictable, conservative option.
Signs that suggest pulp involvement include persistent or severe tooth pain, heightened sensitivity to hot or cold that lingers, swelling or a pimple-like bump on the gum, and pain when biting or chewing. Some teeth may darken in color after trauma or develop chronic discomfort that comes and goes, which can indicate internal changes. In other cases, there may be no noticeable symptoms and problems are found during routine exams or on x-rays.
An accurate diagnosis combines a clinical evaluation with diagnostic tests and radiographs to determine whether the pulp is inflamed or necrotic. Your dentist will consider the amount of remaining tooth structure, periodontal support, and the tooth's role in your bite before recommending treatment. If root canal therapy is indicated, the goal is to remove the diseased tissue and restore the tooth so it can function normally.
Modern root canal therapy is performed with attention to comfort and precision, beginning with local anesthesia to numb the area and allow a pain-free procedure. The dentist gains access to the pulp chamber, carefully removes infected tissue, and shapes the root canals so they can be cleaned and disinfected using advanced instruments and irrigation solutions. Once the canals are thoroughly prepared, they are filled with a biocompatible material and sealed to prevent reinfection.
Some teeth can be treated in a single visit, while others may require two appointments to allow for thorough disinfection when an active infection is present or anatomy is complex. After the canals are sealed, the tooth is rebuilt with a permanent restoration that often includes a full-coverage crown for back teeth to protect against fracture. Follow-up care and routine exams help ensure the long-term success of the treated tooth.
With modern techniques and effective local anesthesia, most patients experience little to no pain during the root canal procedure itself, and the treatment typically relieves the severe discomfort caused by the underlying infection. Mild soreness or tenderness in the treated area for a few days after the procedure is common as surrounding tissues heal, and this is usually controlled with over-the-counter pain relievers or medications when indicated. Your dentist will provide post-operative instructions to help manage any short-term discomfort and support healing.
For patients with dental anxiety or special needs, sedation options may be available to increase comfort and reduce stress during treatment. Good communication with your dental team about your concerns and medical history allows them to tailor pain control and relaxation measures to your needs. Prompt treatment also reduces the risk of worsening infection and more substantial discomfort down the line.
The length and number of visits for root canal therapy depend on the tooth's anatomy, the presence of infection, and whether additional restorative work is planned. Many straightforward cases can be completed in a single visit lasting between 60 and 90 minutes, but more complex teeth or those with active infections may require two appointments to ensure thorough cleaning and disinfection. The treating dentist will explain the anticipated timeline after diagnostic evaluation.
When multiple visits are needed, a temporary filling or medication may be placed between appointments to protect the tooth and reduce symptoms. After the canals are sealed permanently, you will return for the final restoration, which may involve a crown or other protective build-up to restore strength and function. Scheduling and coordination are discussed in advance so you understand each step in the treatment plan.
After root canal therapy, it is normal to experience mild soreness or tenderness for a few days while the surrounding tissues heal, and the treated tooth may feel slightly different as it settles. Maintaining good oral hygiene with gentle brushing and flossing, avoiding hard or sticky foods on the treated tooth until it is fully restored, and following any specific instructions from your dentist all support successful healing. If pain or swelling persists or worsens, you should contact your dentist for further evaluation.
Long-term success depends on placing a durable permanent restoration to protect the tooth from fracture and recontamination, so return visits for crowns or definitive fillings are important. Regular dental checkups and radiographs allow your dental team to monitor healing and detect any signs of recurrent infection early. With proper restoration and routine maintenance, a tooth that has received root canal therapy can function reliably for many years.
Yes, many teeth that undergo root canal therapy remain functional for the rest of a patient’s life when they receive appropriate restoration and routine care. The long-term prognosis is influenced by factors such as how much healthy tooth structure remains, the quality of the root canal fill and final restoration, and overall periodontal health. Addressing restorative needs promptly after treatment helps protect the tooth from fracture and reinfection.
Good oral hygiene, regular professional exams, and prompt attention to new symptoms all contribute to the longevity of a treated tooth. Occasionally, retreatment or surgical endodontic procedures may be recommended if symptoms recur or if previous therapy did not resolve the infection. Your dentist will discuss realistic expectations and follow-up plans tailored to your individual situation.
Alternatives to root canal therapy include extraction of the affected tooth followed by tooth-replacement options such as implants, bridges, or removable prostheses. Extraction removes the infected tooth entirely, but replacing a missing tooth may require additional procedures and long-term maintenance to restore chewing function and preserve surrounding teeth. In some cases, if the pulp inflammation is reversible and caught very early, conservative treatment or monitoring may be possible instead of full root canal therapy.
The decision between treating and extracting a tooth is based on clinical findings, the tooth’s strategic importance, the amount of remaining structure, and the patient’s overall oral health goals. Your dentist will explain the benefits and limitations of each option and help you choose the approach that best preserves oral function and long-term health. When preserving the natural tooth is feasible, root canal therapy is often the most conservative and predictable choice.
Root canal therapy is generally predictable, but as with any medical procedure there are potential risks, including persistent infection, instruments fracturing inside a canal, or difficulties caused by complex root anatomy that can complicate complete cleaning. Occasionally, symptoms can recur and require retreatment or surgical procedures such as an apicoectomy to address infection at the root tip. Your dentist will discuss any case-specific risks identified during evaluation and how they plan to minimize them.
Promptly following post-operative instructions and returning for recommended restorations lower the likelihood of complications related to recontamination or structural failure. If you notice new or worsening pain, swelling, or other concerning signs after treatment, contact your dental office so the issue can be assessed and managed quickly. Regular monitoring through follow-up exams and x-rays helps detect problems early and supports successful outcomes.
Our office emphasizes gentle care and clear communication to make root canal treatment as comfortable as possible, beginning with thorough explanation of the procedure and what to expect. Effective local anesthesia is used to ensure a pain-free experience, and clinicians monitor comfort throughout the appointment while adjusting techniques when needed. For patients with dental anxiety or special needs, sedation options and calming methods are available and can be discussed during consultation.
The goal is to create a low-stress environment where patients feel informed and supported from diagnosis through restoration, and comfort measures are tailored to each individual's requirements. If you have specific concerns about anxiety, gag reflex, or sensitivity, share them with your dental team so they can propose appropriate strategies and accommodations. At Lesley Holloway the Dentist we prioritize patient comfort and individualized care during every step of treatment.
Quick Links
Contact Us